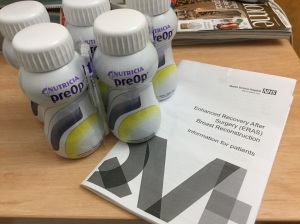
I slept surprisingly well the night before surgery and was woken from a deep sleep at 6am and asked to drink the remaining 2 carbohydrate drinks within half an hour. At that time in the morning they tasted twice as sweet and were pretty hard to stomach but at least it was fluid which meant I wasn’t left feeling thirsty. I took a shower, donned my hospital gown and slipped into my green knee high compression socks (photo as promised).

It wasn’t long before I was called down to the theatre area. I was taken to a single bay with a bathroom where more paperwork was completed and I was looked after by one of the nurses – I think her job was to keep me warm and calm. She did this by wrapping me in a silver blanket and talking to me about Christmas. I guess for her, being in a room with someone with no hair and covered in what looked like tin foil, the turkey resemblance was too great to talk about anything else.
Before long I was being strolled down a corridor and into the anaesthetic room of Operating Theatre 6. Here I was asked to lay on a bed while my particulars were checked one final time. A cannula was inserted into the back of my hand and an oxygen mask placed over my mouth. I took a few deep breaths and the next thing I knew I was somewhere else – I can’t be sure where I was but it wasn’t the room I had just been in and it wasn’t Kansas. So it was either recovery or back on the ward in the step down unit. From what I have since been told, I was in theatre for 9-10 hours and in recovery for 2-3 hours after that.
The evening events are quite a blur, I remember lots of poking around my chest, some strange noises, taking sips of water through a straw, my blood pressure being taken and various voices coming and going. There was pain in my abdomen but no pain at all around my breast area. I recall being asked 2 questions that evening….. ‘Do you want to have a look?’ (at my boobies) and ‘do you want to speak to your husband?’ The answer to both questions were the same, a very firm ‘no’. Not because I didn’t want to, I just didn’t have the energy to do either.
The first real memory I have is around 6am the following morning when I was visited by the night doctor at the end of her shift. She came and stood next to my bed and when I looked at her I realised I had seriously bad vision. It was similar to the experience I had when on chemo so I wasn’t overly concerned. It was at this point that I became conscious of the various paraphernalia that was now being used on me. Starting from my feet travelling up, these were as follows;
My green decompression stockings
Flowtron boots – despite sounding like vital fashion attire for a 1970’s disco diva, these are actually a proper medical piece of equipment that massaged my calves to help prevent DVT.
Blood pressure cuff on my right thigh
Urinary catheter
3 drains each about the size of a pint glass. The purpose of these are to drain away excess fluid around the surgery site so I had one for each breast and one for my abdomen.
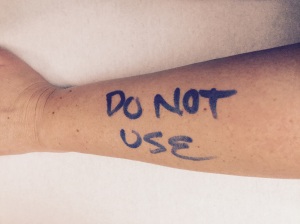
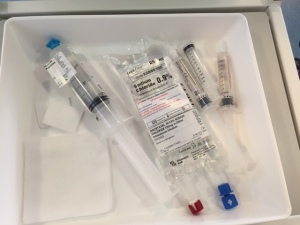
5 cannula’s – these were all in my right hand. I have no idea what they were all for but for now they were behaving and I was relatively pain free
Finger Pulse Oximeter – to measure pulse and saturation levels
Nasal cannula – one of those plastic tubes to give you oxygen
I also had a heat blanket over the top of me.
I was however missing one item and that was my central line. We had agreed the evening before surgery to remove it as it was just going to get in the way.
So day one went pretty well. Early in the morning the Flowtron boots and the heat blanket were removed along with 2 of the cannula’s. I was visited by one of the assistant surgeons who told me they were very happy with how the surgery had gone. He explained that they discovered my abdominal muscles were separated, probably from being pregnant. So as well as the planned surgery they also rectified this by pulling the muscles back together and stitching them up – reunited once more. I was given the all clear to have something to eat which basically meant that they didn’t see the need for me to go back to theatre. I celebrated with a bowl of cornflakes.
Later in the morning the blood pressure cuff, finger pulse monitor and 2 more of the cannula’s were removed, the nurse also put on my bra and a binder on my stomach. This is basically a corset type contraption to hold everything in but after enduring such intense stomach surgery it really wasn’t very welcome. I had been handed a PCA – Patient Controlled Analgesia, when I pushed the green button mophine made is way to the last remaining cannula and relieved most of the pain. It was put to good use that day but made me so spaced out that I probably dribbled on more than 1 occasion.
Half an hour before lunch was served my nurse came along and announced that it was time to try to get out of bed. The process of sitting up and maneuvering myself to the side of the bed was enough effort to leave me gasping for breath and scrambling for the PCA. I took a few minutes to regain my composure before final taking the plunge and started the process of standing. Well, I say standing but it was more of a bizarre yoga pose as I had to hold one hand across my stomach and use the other hand to support myself using the nearest stable object. To add to this I couldn’t fully stand up due to the pain so ended up bending forward with my bum sticking out. I then shuffled my feet to the chair that was all of 20cms away and turned the 90° that was required before I could sit down. A few more deep breaths and I slowly took the plunge. I wondered who was lowering the seat as I tried to make a connection between it and my backside but I finally made it and it was OK. I stayed there for a couple of hours before returning to bed exhausted.
The afternoon bought along the physio team, who gave me gentle arm exercises, the pain relief team, who gave me a few options to keep the pain under control and regular visits from my nurse who continued to check the usual ‘obs’ (blood pressure, body temperature and saturation levels).’ She also checked my new boobs at the same time – a gentle touch of each to ensure they were warm and also a listen on an ultrasound doppler to check that the blood was flowing through the blood vessels as it should be – this was the strange noise I had heard through the night before as it was checked every half hour.
Early evening bought another venture into my chair and an objection from the vein homing the cannula. By 8pm it won the fight and I lost my beloved morphine. I was switched to liquid morphine instead and was high and happy once more. Here’s the mophine induced selfie just to prove that point!

Trust me, the smile didn’t last long but I’ll write about that at a later date. All you need to know for now is that I came home on Sunday (day 5) and all is as well as it can be.